- What is Interoperability in Healthcare?
- Understanding the Levels of Healthcare Interoperability
- Foundational
- Structural
- Semantic
- Organizational
- Importance of Interoperability in Healthcare
- Importance of Achieving an Interoperable Healthcare IT Infrastructure
- Examples of Interoperability in Healthcare
- Benefits of Healthcare Interoperability
- Enhanced Patient Care
- Continuity of Care
- Improved Efficiency
- Cost Savings
- Patient Empowerment
- Public Health Initiatives
- Streamlined Administrative Processes
- Better Data Analytics
- Challenges of Interoperability in Healthcare
- Data Governance and Quality Assurance
- Technological Heterogeneity
- Regulatory Compliance
- User Training and Education
- Interoperability Governance
- International Standardization
- Patient Data Matching and Identification
- How to Achieve Interoperability in Healthcare IT?
- Define Clear Objectives
- Analyze Existing Systems
- Adopt Standards
- Make Privacy and Security a Top Priority
- Build a Seamless Patient Journey
- Future of Interoperability in Healthcare
- Attain Interoperability in Healthcare with Appinventiv
- FAQs
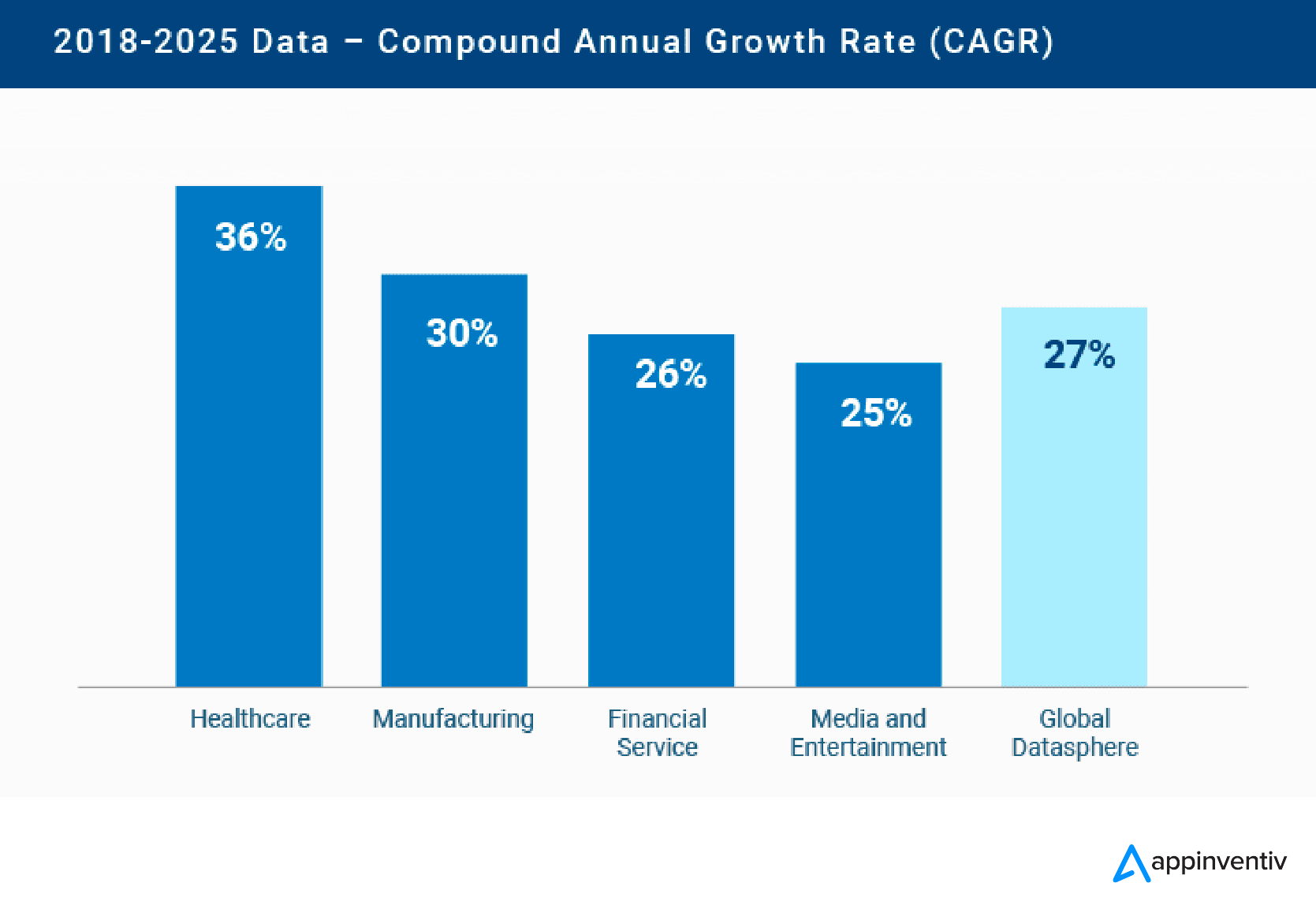
Healthcare is one of the most innovative sectors in terms of data development. The sector currently accounts for 30% of the entire global database stream and is expected to rise to 36% by 2025.
It is important to note that healthcare has been growing at a faster rate than other major sectors, including 6% faster than manufacturing, 10% faster than finance, and 11% faster than the media & entertainment industry. With the rising volume of this data, the importance of medical information in improving the quality of healthcare becomes obvious.
Nevertheless, it clearly presents the paradox of progress because, on average, doctors spend 18.5 million hours every year doing the most basic data collection administration stuff. This significant investment of time and energy prompts a crucial concern – the necessity of attaining interoperability in healthcare.
This article will discuss why we need to make health IT interoperability a priority, looking at the complex world of medical data and how it can simplify tasks for healthcare workers while addressing the challenges that hamper the way of attaining interoperability in healthcare.
What is Interoperability in Healthcare?
The ability of an electronic healthcare system to communicate seamlessly with other computers or software systems from various healthcare providers or hospitals is referred to as interoperability in healthcare. It goes beyond interconnectedness and allows the sharing and opening of health information across pharmacies, labs, clinics, hospitals, and hospices.
Healthcare providers are required to use strict data standards to protect Patient Health Information (PHI) as it is extremely sensitive. Adhering to such regulations provides a guarantee of safe data transfers across the healthcare environment.
Some key aspects of health IT interoperability include:
- Fast Healthcare Interoperability Resources (FHIR): FHIR provides a structured plan for sharing digital health data. It’s made to be changeable and used in many situations with various health information.
- Interoperability Standards: These rules explain the technical terminology and references needed for sharing healthcare information. It makes sure that systems can communicate with each other properly.
- Information Exchange Workflow: With safety and privacy in mind, interoperability solutions help to share health information. This exchange happens between different parties, like doctors, patients, and external web developers.
- Uses of Information Exchange: IT healthcare solutions that work together can assist doctors in getting the most recent science-backed medical advice. They can improve active health upkeep for their patients. Plus, these systems can make it easier to work together with other health care providers.
- Privacy and Security: Privacy and safety of health details are key to effective sharing. Interoperability needs safe sharing as it uses sensitive information. This info needs to have the utmost privacy and security.
Understanding the Levels of Healthcare Interoperability
In the field of healthcare interoperability, there exists a hierarchical structure where each level of healthcare interoperability plays a unique role in enabling smooth data exchange. The Health Information Management Systems Society (HIMSS) has categorized health IT interoperability into four distinct levels: foundational, structural, semantic, and organizational.
Let’s explore healthcare interoperability stages in detail:
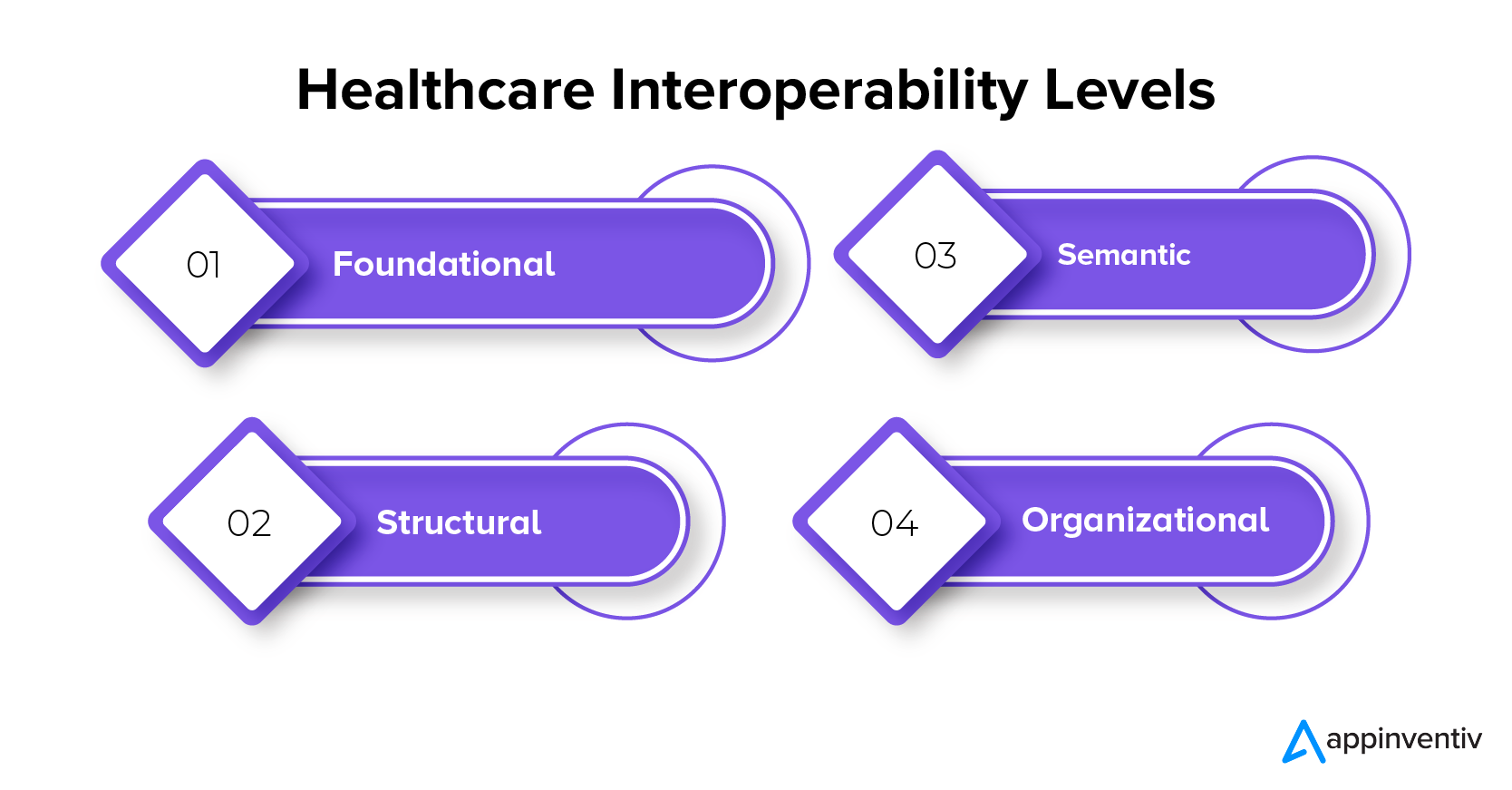
Foundational
At this phase, a foundational framework is set for ensuring secure communication across varied systems or applications. However, at this level, the data information technology solutions are unable to completely comprehend the healthcare data they receive. So, the incorporation of further interoperability levels becomes imperative for processing data and extracting significant insights.
Structural
When it comes to structuring data sharing, the focus lies on defining the format, syntax, and organization. Standards like Health Level 7 (HL7) offer direction on message structuring. While structural interoperability allows healthcare data interpretation between systems, the content within a structured message may lack full standardization, which hinders comprehensive understanding between systems.
Semantic
Semantic interoperability involves utilizing medical terminologies, nomenclatures and ontologies to establish a mutual comprehension of medical concepts across various systems. This not only enables the exchange and interpretation of healthcare data but also ensures its meaningful utilization through data information technology solutions. For instance, SNOMED serves as a general-purpose language, while domain-specific terminologies such as LOINC cater to laboratory observations and IDMP is designed for medicines.
Organizational
At this highest level, governance, policies, social factors, legal aspects, and organizational deliberations are integrated for healthcare interoperability. This involves a comprehensive strategy to enable the secure, smooth, and prompt transmission of healthcare data among various organizations, entities, and individuals. To attain organizational interoperability, uniform business processes, and workflows are essential, enabling the seamless delivery of healthcare services across diverse institutions.
Importance of Interoperability in Healthcare
The importance of healthcare data interoperability is highlighted by potent numbers, indicating its significance in today’s health world. An impressive 64% of all doctor visits, 70% of hospital stays, and a whopping 83% of all drug prescriptions are deeply tied to the smooth sharing and access to health information. Also, a notable 71% of total healthcare costs and a big 93% of Medicare costs are crucial parts of the health use scenario.
These numbers highlight how far interoperability can go in improving the efficiency and affordability of healthcare services. Interoperability gives clinicians full access to patient data, which helps them make informed decisions and provide more customized and successful care. The linked relationship between patient visits, hospital stays, and prescription handling shows the demand for a united data ecosystem that goes beyond organization limits.
In complex healthcare finance, achieving interoperability becomes essential in optimizing resource allocation. Statistics emphasize that a significant part of healthcare spending, especially within Medicare, relies on the seamless sharing and access of health information. Adopting interoperability allows healthcare systems to streamline processes, minimize duplications, and ultimately lower expenses while enhancing patient results.
The data essentially highlights the unquestionable significance of healthcare interoperability as a key element. It tackles present healthcare utilization and spending challenges and also promises a more interconnected, patient-focused, and cost-effective healthcare system in the future.
Importance of Achieving an Interoperable Healthcare IT Infrastructure
The need for a strong and adaptable health IT infrastructure highlights the importance of achieving interoperability. This is crucial in creating a healthcare system that is transparent, efficient, and promotes informed decision-making. It helps reduce duplication, drive payment reform, and transform care to focus on accessibility and overall well-being. The ultimate goal is to build a health system that prioritizes individual empowerment, personalized treatment, and speedy disease cure.
Interoperability is not just a technological challenge. It is about easily and appropriately sharing health information to support various needs. We need to provide consumers, providers, payers, and employers with information about quality and service utilization to ensure cost-effective care. Physicians rely on health IT to enhance patient care, and there is a growing interest in empowering individuals to take an active role in their healthcare journey.
With the advancement of technologies, like wearables and telehealth, a more connected and adaptive environment is possible. The aim is to establish a learning health system that benefits both the present and the future. Such a system can lead to reduced healthcare expenses, better overall population health, increased consumer empowerment, and ongoing innovation.
Also Read: Top Healthcare Trends that will Redefine the Industry
Examples of Interoperability in Healthcare
Healthcare data interoperability means different information setups, tools, and groups can easily swap and use health data. Let’s check out some interoperability in healthcare examples:
- Digital Health Records (DHRs) and Health Data Swap (HDS): DHR systems provide safe swapping of patient details with other care providers and HDS networks. This allows for easy movement of patient information between different healthcare environments.
- Fast Health Data Transfer Guidelines (FHIR): FHIR is a guide for sharing electronic health records. It helps systems like electronic health records (EHRs) communicate with each other. It also supports health info from different places, like mobiles and wearable devices.
- Online Healthcare and Patient Check-ups: Connected platforms help monitor patients from a distance and facilitate the sharing of details between patients and healthcare providers. This leads to virtual doctor visits and long-distance handling of lasting medical conditions.
- Medical Assistance Software (MAS): Functional MAS offers medical personnel immediate links to established health advice, medication alarm notifications, and patient-tailored suggestions. This boosts healthcare quality and guarantees patient safety.
You may like reading: How Mobile Apps Are Transforming the Healthcare Industry?
Benefits of Healthcare Interoperability
Healthcare interoperability helps everyone involved in the healthcare system. Let’s learn about some important benefits of healthcare interoperability for patients, healthcare workers, doctors, and the overall healthcare sector.
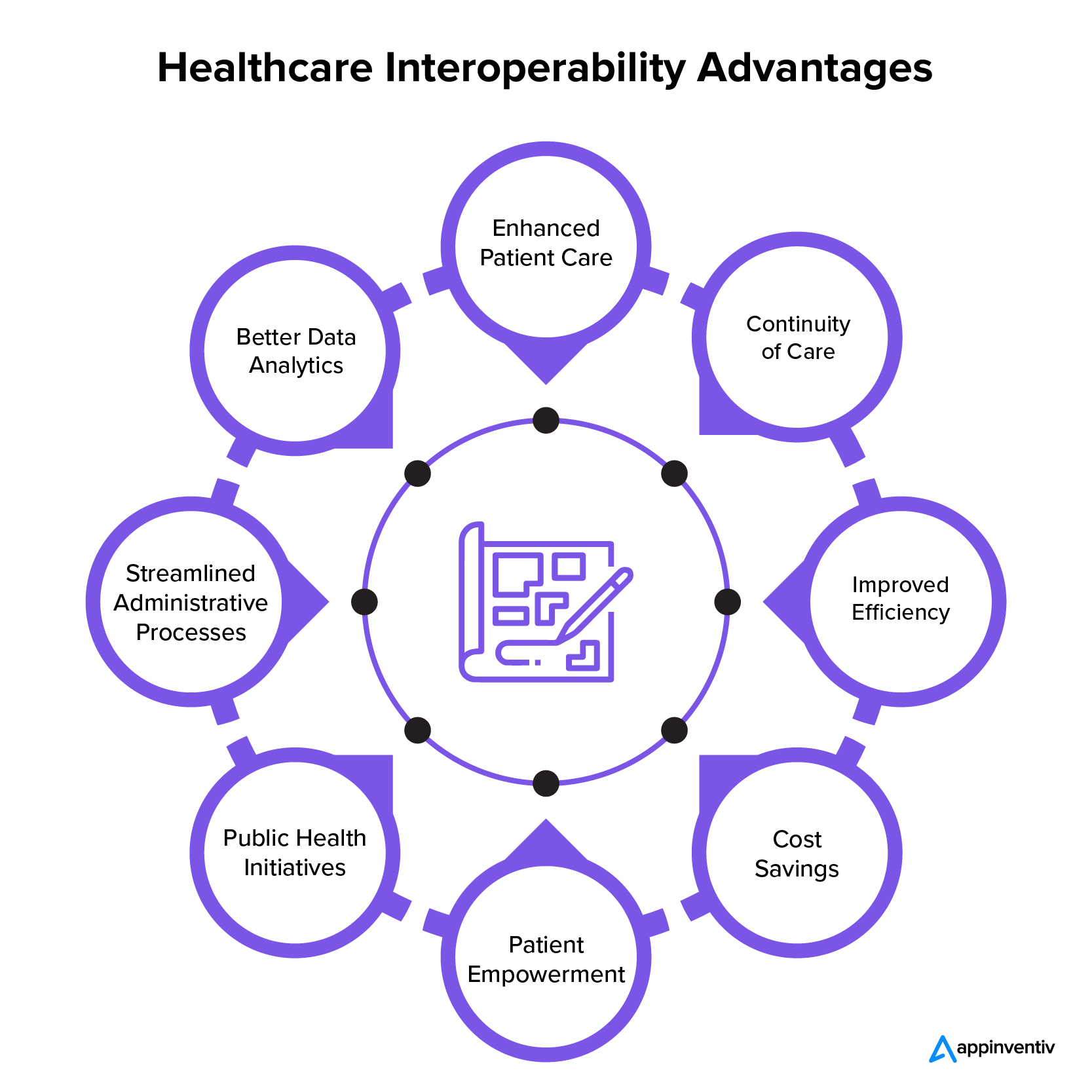
Enhanced Patient Care
Interoperability is the backbone for healthcare providers, granting them a holistic and current understanding of a patient’s medical background. This key capability empowers well-informed choices, diminishes potential medical mistakes, and enriches the overall quality of patient care.
Continuity of Care
Many patients require treatment from different healthcare professionals across other locations. Interoperability plays a crucial role in facilitating the smooth flow of health information, thus guaranteeing consistent care delivery and averting any disruptions in treatment.
Improved Efficiency
Making data sharing smoother between various health systems reduces typing work, paperwork, and repeat tests. This effective approach not only saves time but also lessens the chance of mistakes linked to manual tasks.
Cost Savings
The cost benefits of healthcare interoperability include eliminating repetitive and rule-based tasks, lessening mistakes, and boosting the smooth run of things. It makes the best use of resources and aids in managing healthcare spending.
Patient Empowerment
Empowering patients through interoperability grants them expanded access to their health information, fostering transparency and active engagement in healthcare choices. This approach further promotes adherence to treatment plans and empowers individuals to assume control over their well-being.
Public Health Initiatives
Interoperability plays a crucial role in advancing public health initiatives. It facilitates the prompt exchange of data concerning disease outbreaks, health trend monitoring, and the implementation of preventive measures – all working towards enhancing population health management.
Streamlined Administrative Processes
Automating administrative tasks in health contributes to a reduction in the workload for medical professionals. This involves streamlining billing processes, managing insurance claims, and executing other administrative functions, ultimately enhancing the efficiency of workflow.
Better Data Analytics
Health data interoperability enables in-depth data analytics, offering valuable perspectives into public health, treatment efficacy, and patterns within the healthcare landscape. This method, rooted in data, facilitates informed decision-making and long-term strategizing.
Challenges of Interoperability in Healthcare
Health IT interoperability faces several challenges that hinder the seamless sharing and use of health information across different systems. Some of the key challenges of interoperability in healthcare include:
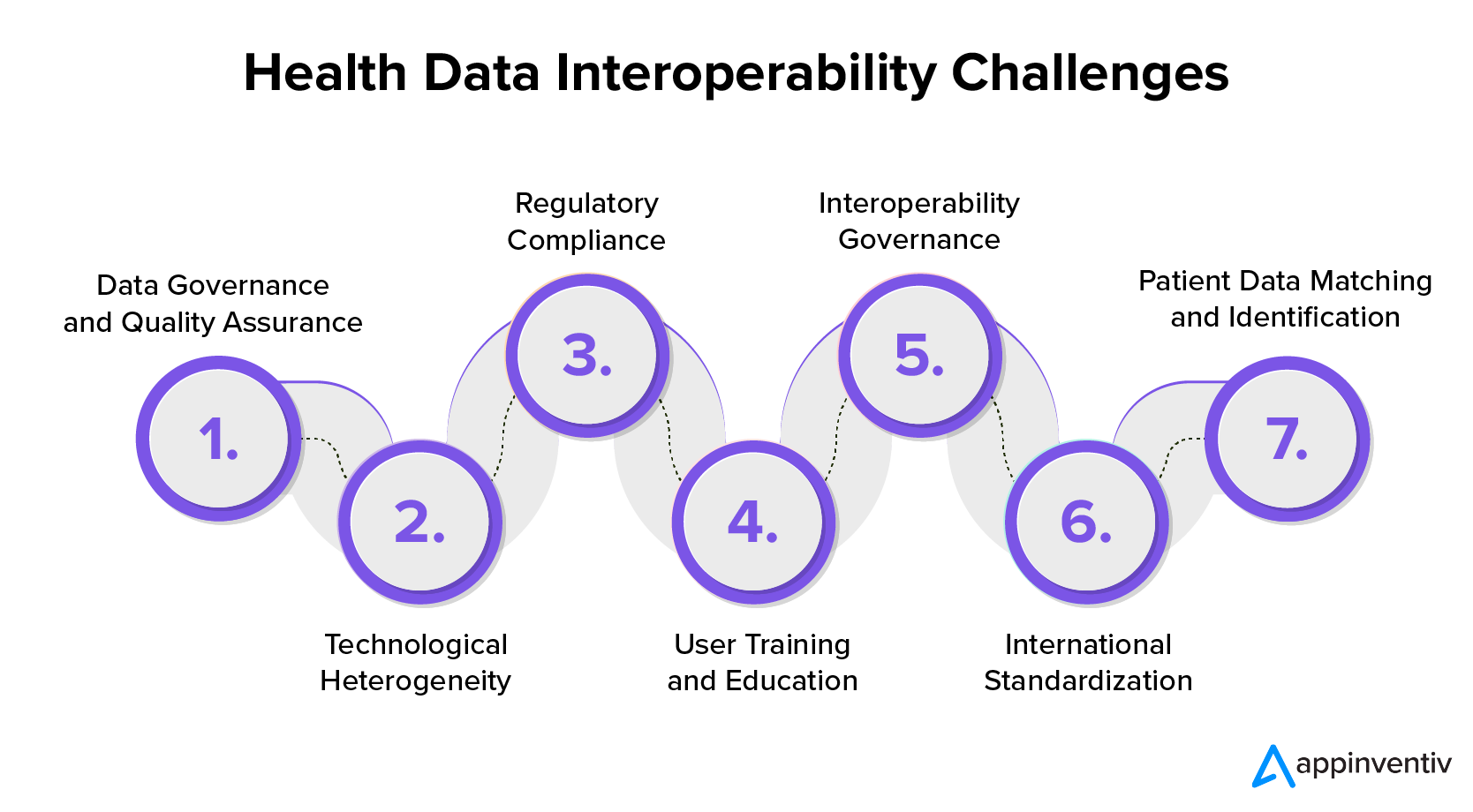
Data Governance and Quality Assurance
Ensuring the effective governance and quality assurance of healthcare data is essential for achieving seamless interoperability. Lacking standardized data governance can lead to challenges concerning accuracy, integrity, and uniformity, which can affect the dependability of exchanged data.
Technological Heterogeneity
In healthcare, technological heterogeneity poses a notable challenge. This issue arises due to the use of diverse techniques and systems supplied by various vendors within the industry. The presence of incompatible technology stacks and architectural differences can hinder seamless communication between systems, thus causing complications.
Regulatory Compliance
Healthcare regulations like HIPAA in the United States make it difficult to achieve interoperability. These standards add extra complexity, and we need careful thinking and actions to follow these compliances while sharing data.
User Training and Education
Introducing interoperable systems into healthcare often requires educating and training healthcare professionals to utilize new technologies effectively. The learning curve involved in these transitions might hinder their acceptance and could demand significant investment in training initiatives.
Interoperability Governance
Establishing robust governance frameworks for interoperability initiatives is essential. This involves tackling concerns surrounding data ownership, access controls, and accountability to facilitate seamless collaboration among various entities within the healthcare ecosystem.
International Standardization
To allow smooth operation globally, businesses need to stick to international rules. Differences in these rules from country to country could block the easy flow of health info worldwide.
Patient Data Matching and Identification
Ensuring precise matching and identification of patient records across diverse systems poses a continual challenge. Mismatches or inaccuracies in patient identification can have severe repercussions that can jeopardize the credibility of shared health data.
How to Achieve Interoperability in Healthcare IT?
Ensuring healthcare information systems can work together smoothly requires a strategic plan with clear steps to enhance data exchange and ultimately elevate patient care. Here are the steps to attain interoperability in healthcare:
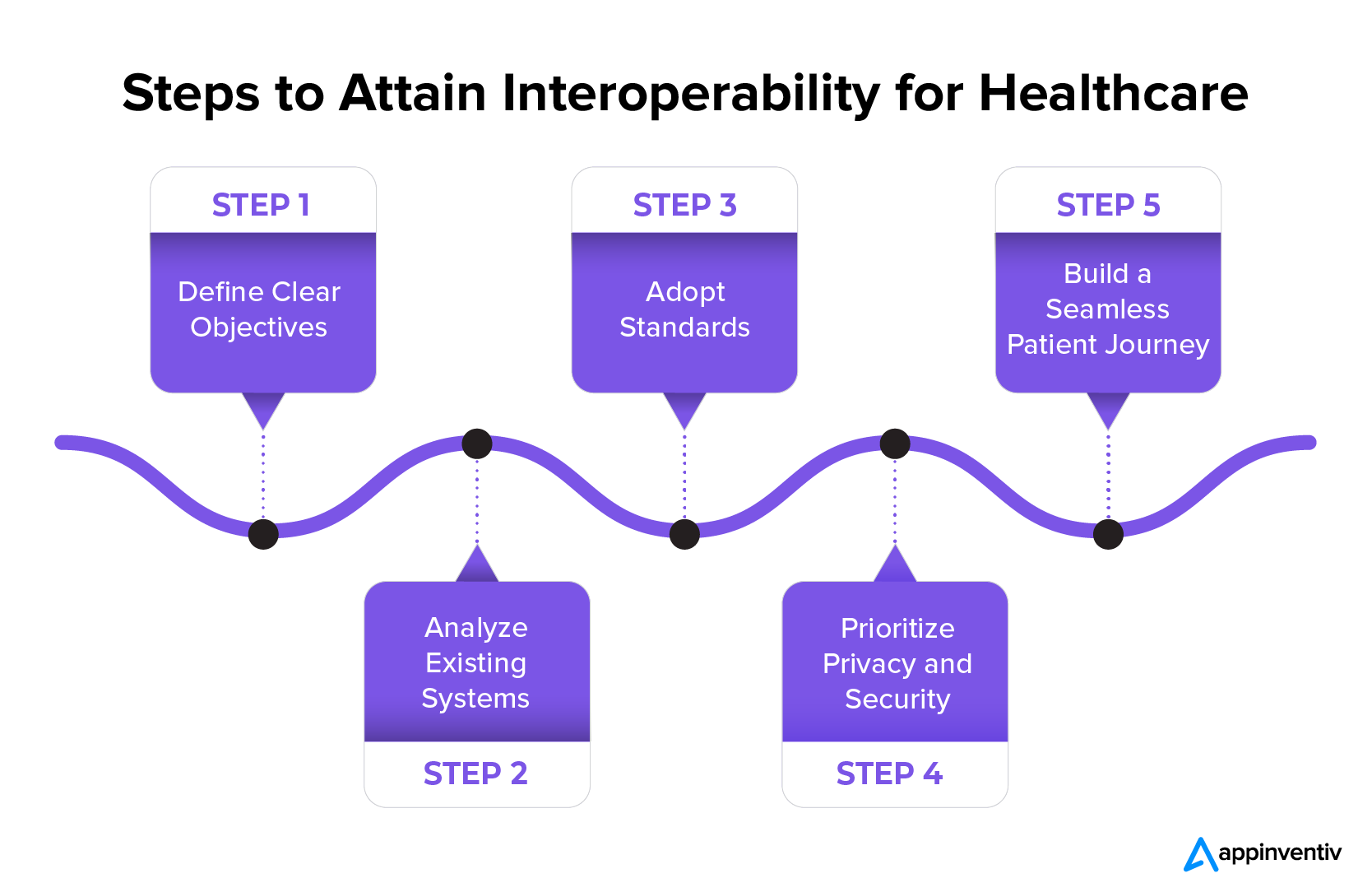
Define Clear Objectives
Defining clear objectives for interoperability is crucial in the healthcare system. This involves determining the desired interoperability level and establishing a practical timeline for its execution. Objectives may encompass various targets such as integrating different hospital departments, attaining specific healthcare interoperability stages(e.g., Level 2 or 3), or enhancing current interoperability capacities.
When outlining the strategy, it’s essential to comprehensively consider all factors, including human resources, required software, and potential technological integrations. Emphasizing compliance with healthcare regulations, particularly those related to safeguarding patient data such as HIPAA, is essential in goal-setting to uphold the confidentiality of exchanged information.
Analyze Existing Systems
Achieving health IT interoperability calls for a comprehensive evaluation of current data-sharing processes and existing software systems. Establishing interoperability within facilities already employing EHR or HIE is essential, so exploring avenues for expansion and integration within these systems is crucial.
Additionally, conducting a detailed technical analysis of all software and aligning it with the envisioned level of interoperability lays the groundwork for effective planning. Seeking expert opinions, when necessary, can offer valuable insights. Meanwhile, for departments still reliant on outdated methods, the introduction and adoption of EHR serves as a foundational step, ensuring a seamless transition from manual to digital data management and sharing.
Adopt Standards
The implementation of standards plays an important role in guaranteeing smooth data exchange. By outlining data format and technology standards, a cohesive approach is established for various software and applications. Fast Healthcare Interoperability Resources (FHIR) serves as an open-source standards framework, streamlining the exchange of healthcare data between systems.
Standardizing the organization’s terminology, with the assistance of systems such as the ICD-10 medical classification, fosters uniformity and comprehension. The incorporation of these standards ensures that systems can efficiently analyze shared data, consequently improving interoperability.
Make Privacy and Security a Top Priority
Understanding that a patient’s health details are delicate, businesses must put privacy and safety first. Organizations uphold laws like HIPAA that safeguard patient data during the sharing process. This means making sure all systems follow these rules and carry out routine training sessions for the staff and doctors. It’s essential to create an alert and rules-following environment to keep patients’ data safe and intact during the whole data transfer journey.
Build a Seamless Patient Journey
The main aim of interoperability is to enhance the patient’s journey and experience. It’s crucial to comprehend patient behaviors at all interaction levels to accomplish this objective. A healthcare CRM that complies with HIPAA regulations serves as a valuable asset in documenting patient engagements at various touchpoints.
Integrating the CRM with the EHR enables the smooth transfer of recorded data, resulting in a comprehensive overview of the patient’s entire journey. This integrated method significantly enriches the overall patient experience, commencing from the initial touchpoint, such as scheduling appointments or even before, ensuring a holistic and patient-centered approach to healthcare.
Future of Interoperability in Healthcare
The future of interoperability in healthcare looks promising with the implementation of emerging technologies and enhanced interoperability standards like FHIR, promoting seamless data exchange.
For instance, blockchain is designed to address security concerns, ensuring trustworthy data sharing. Improved APIs will foster efficient communication, enabling a patient-centered approach to personalized care. The integration of AI and ML in healthcare promises informed decision-making and personalized treatment plans. The growth of the IoT in healthcare expands data interoperability, incorporating wearables and remote monitoring.
Government regulations emphasize standardized data exchange and global health information sharing. Currently, healthcare initiatives are focused on integrating telehealth and virtual care, prioritizing interoperability between digital platforms and conventional systems. Cybersecurity is essential in safeguarding patient information during exchanges.
The future of healthcare interoperability envisions a more connected, intelligent, and secure landscape, prioritizing improved patient experiences and outcomes.
Attain Interoperability in Healthcare with Appinventiv
Interoperability in healthcare IT is essential since it improves patients’ outcomes, service delivery, and financial health. Consequently, healthcare institutions should consider the challenges that may arise and take other regulatory endeavors to establish a more interoperable health information system that effectively delivers improved care outcomes.
When looking for the best healthcare IT consulting services to attain interoperability, you can consider partnering with Appinventiv. We have a proven track of building advanced healthcare applications for businesses worldwide.
Our portfolio demonstrates effective solutions for medical businesses, including YouCOMM, which increased the nurses’ response time by up to 60% over 5+ hospital chains in the US.

Furthermore, millions of people have embraced Soniphi, an e-health app that records user’s voices for complete health analysis, demonstrating the significance of our innovative approaches in software development.
Interested in building similar solutions and advancing your health IT interoperability journey? Opt for our healthcare software development services now and see your business reach greater heights.
FAQs
Q. Why achieving an interoperable healthcare IT ecosystem is paramount for businesses?
A. An interoperable healthcare IT ecosystem is crucial for businesses as it facilitates information exchange, collaboration, and seamless communication among healthcare entities. This effectiveness improves patient care, enhances operational effectiveness, and ensures compliance, making it essential for successful healthcare experiences.
Q. Are there specific standards or protocols governing Health information exchanges and interoperability?
A. Standards like Health Level 7 (HL7) and FHIR serve as the governing bodies for the exchange of health information. They play a pivotal role in ensuring compatibility and seamless communication between different health systems.
Q. Can interoperability help reduce medical errors?
A. Interoperability in healthcare greatly reduces medical errors by granting healthcare providers access to thorough and precise patient data. This enhances decision-making and advances patient safety.


How Much Does it Cost to Build a Custom Dental Practice Management Software?
In recent years, dental practices have shifted away from manual, paper-based systems and embraced advanced software solutions. This change boosts efficiency, enhances patient experiences, and improves data management. While dealing with patient data, dentistry has ditched old-school methods like physical charts, appointment books, and manual billing. They’ve leveled up with a high-tech data handling &…

EMR Integration in Healthcare Systems - Benefits, Features, Process, Costs
EMR integration, having proved its worth in the healthcare space with improved workflows, better patient engagements, and lowered operational costs has built itself a projected market share of USD 20.7 billion. Eventhough a range of hospitals swear upon the benefits EMR system integration has garnered them, the adoption level digital healthcare industry anticipated has still…